As some of you may already know from reading my bio or from talking to me, I currently have a broken heart. Not in the lovey dovey way, but in the actual physiological way. I have a condition called Atrial Tachycardia (AT), and it’s really irritating me.
I was diagnosed quite suddenly with AT in 2005, Halloween to be exact. I had been at work all day taking care of my marketing peeps, promoting people, moving people.. all the regular stuff. I was having some pain in my chest, but really didn’t think anything of it. I, like many others, chalked it up to stress or a pulled muscle and kept on going. It was only after the pain didn’t go away that I decided maybe I should see a doctor. I stopped in to urgent care at the U of MN on my way home just to be safe. Wow, was I surprised at how quickly they got a doctor when I said I was having chest pain, no sitting around the waiting room for me!
I actually felt a little silly, thinking “all this for a pulled muscle or anxiety?”
They were very thorough, in fact I was getting a little irritated that they weren’t just dismissing me. They insisted on running a test to check for a chemical that shows up if you’ve had a heart attack, they hooked me up to a Heart Rate Monitor (HRM), they poked, prodded, ran EKG’s and had me wait around to see a specialist. Once the cardiologist saw me, he said that he had some concern about my EKG. There seemed to be an irregularity in the way my heart was beating, and that the rate was a bit too fast. He asked if I would be willing to wait and have a stress test in the morning once the labs opened up. Since it was already very late, I agreed. At this point I was getting a little concerned myself.
In the morning, the lab opened up and they sent me down for a stress test. Not the normal standing one, because they were concerned I would have an “episode”, I had to do the bicycle stress test that’s done while lying down. The test itself really wasn’t that bad, I just had to pedal the bike and keep a pace that lit up a light on the machine.
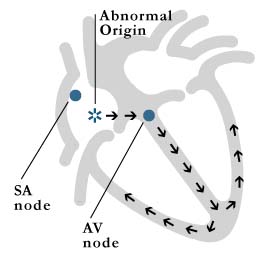
Once he read the results, the cardiologist pulled me and my partner aside. The good news was that I hadn’t had a heart attack, but there was an issue. Apparently after looking at the test results he had identified that my heart was beating in the opposite way that a normal heart does. When I was resting, my heart was in a rhythm like I was in the midst of a full on exercise class. The atrium was sending a signal when it shouldn’t and the end result was that not only was my heart rate too fast, but the wrong part was sending a signal to beat. I had tachycardia with an arrhythmia (sometimes referred to as tachyarrhythmia), and I needed to come back and see an Electrophysiologist (EP). An EP doctor is a cardiologist whose sub specialty is the electrical function of the heart.
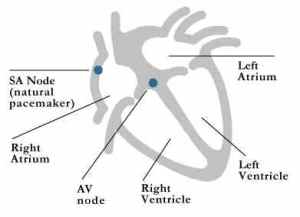
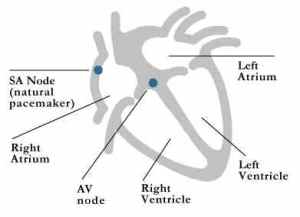
Normal Heart Function
I went to see the EP doctor, Dr. Scott Sakaguchi, on a follow up appointment. He was very nice, seemed super smart, and he clearly knew what he was doing. He told me about how a normal heart beats, and how mine was beating in comparison. A normal heart has a natural pacemaker called the SA Node, which is supposed to send the signal to beat.
My heart was short-circuited and sending too many signals. It needed to be fixed, my heart was already slightly enlarged, a side effect of tachycardia. He thought that I had probably had the condition for years, but had gone undiagnosed because my heart rate really wasn’t high enough to raise a red flag for anyone. The heart rate was probably dismissed by other doctors because of my previous obesity. We talked about solutions, for a first round of treatment there was either drug therapy or Radio-Frequency Ablation (RF Ablation). As a very last resort they would consider shutting down my heart completely and implanting a pacemaker to do the work that my heart couldn’t do. We weren’t ready for that yet, it just seemed too extreme.
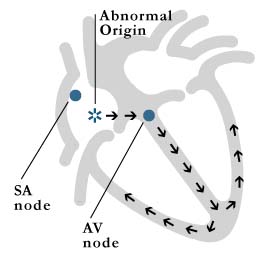
Atrial Tachycardia
Drug therapy was a very common form of treatment, and specifically we talked about Beta-Blockers like Atenolol or Metoprolol. Beta Blockers work by creating a chemical reaction in your body that blocks the effects of adrenaline allowing your heart to relax and beat more slowly. The most common side effects of these drugs are fatigue, dizziness or weight gain. Although I wasn’t completely against drug therapy, it seemed like it would be more appropriate in someone who didn’t need a long term treatment plan. I just couldn’t see myself taking drugs for the rest of my life, I was only 37 at the time.
Radio Frequency Ablation is a non-surgical treatment for arrhythmias and other heart issues. Catheters are inserted into the veins in the groin and threaded up into the heart with the guidance of x-rays or magnets. Once the catheters are inside of the heart, the doctors do an EP study to determine which part of the heart is sending faulty signals. Once the doctors map the heart and find the problem spots, they use low temperatures to burn the heart tissue. Believe me, its sounds A LOT worse than it really is. The damage to the heart is minimal, and doesn’t have long term adverse effects, it simply is supposed to stop the signal from being sent from the incorrect part of the heart. Ablation is about 95% effective in most patients. There is only a one night stay in the hospital, and is done under sedation in most cases.
RF Ablation seemed like the route to take, it was non-surgical and very successful in use for treating tachycardia and other arrhythmias. I was scheduled for my first ablation to occur on 11/21/05.
I was preparing for the ablation, my family had come into town. We were all a little worried about it, and didn’t really know what to expect. The day before I was scheduled to go into the hospital, I had an episode. I was sitting on the couch after just having gotten up on a lazy Sunday morning, I hadn’t even had my first cup of coffee yet. My sister called and I was talking to her on the phone, when suddenly I passed out. Of course, I didn’t realize it. I woke up confused and feeling like my head was shaken loose. My partner was standing over me, I could hear her quickly telling my sister that we had to call 911 because I passed out. I passed out again, my partner did indeed call 911. I woke again and was still really confused and didn’t understand what was going on. The EMT’s got to the house, hooked me up to some machines, put me in the ambulance, and took me to the U of MN. My sister and mom met us at the hospital. I was wheeled into the emergency room and hooked up to many monitors, given another IV (apparently they need two- one for the drugs and one for back up, who knew?). All the while people rushed around and said things like “stat” and phrases you only hear on TV shows like, “I need a CBC Chem-7” and “a shot of epi”. It was all very surreal. I was hooked up to a heart monitor, and my family’s eyes were glued to it. At some point I passed out again, when I woke up I remember seeing my mother’s face and thinking that I had never seen her so worried, or maybe terrified is a better word. Apparently my monitor had flat lined.
I’m not sure if I passed out again after that, but the doctors explained that I was having episodes of syncope. The heart pauses as if to reset itself, the patient passes out briefly and then wakes up. This is sometimes followed by another episode of passing out. Syncope in itself isn’t life threatening (even though very scary) because the person regains conscienceness, but can be an indication of a condition that could later cause sudden death. They admitted me to the ICU for observation, but I didn’t have any more instances of syncope after that.

Typical EP Lab
The next day, the EP study and ablation took place as planned. I was brought into the lab (yes, it’s more like a lab than an operating room), prepped and given a sedative. Since I wasn’t fully asleep during the procedure, I would wake up sometimes and watch what was going on. It was really an odd experience. I could see the computer monitors, and the images of the catheters being threaded into my heart, but I couldn’t really feel it- just a slight movement or pressure inside of me. Sometimes when they were mapping (or pacing) I could feel my heart speed up. They would then give me more sedative and I would fall back to sleep, this went on for hours and hours. When I woke up at the end of the day, the doctor told me that he had found several areas of my heart that were sending incorrect signals, but unfortunately the burning hadn’t gotten rid of the arrhythmia or slowed down my heart rate. I spent the rest of the night in the hospital, completely immobile after the procedure.
The procedure had lasted about 13 hours, and I was back at square one. I was disappointed, sore, sick from the sedation, and not cured.
I explain this in such detail to give you an idea of what it was like, not because it’s terribly interesting, but because this is only one of the five ablations that I have been through. Shortly after this ablation, I had another in January, 2006, also unsuccessful. After the second unsuccessful ablation here in MN, my doctor started speaking to a well known doctor at the Cardiac Arrhythmia Research Institute in OK. Doctor Warren Jackman is world renowned as one of the leading EP researchers. He pioneered many different types of ablation techniques and was respected in the EP world as a leader in this type of medicine. My doctor in MN sent all of my files to Dr. Jackman and asked him to take my case. Dr. Jackman agreed, and I was scheduled to go to C.A.R.I. to have my third ablation. In May of 2006 I traveled to Oklahoma City and underwent a slightly different kind of ablation. The technology was basically the same, but the catheters that they used were much more powerful than those used here in MN. In fact, they burned so much hotter that the catheter actually sprayed water during the procedure to cool down the burn site. The procedure in OK City left me very battered, but it appeared to work. I was sent home with a gross of blood thinners (so that I didn’t stroke out) and strict orders to take it easy. I got home and did just that, I was incredibly relieved, and felt so much better. I was able to resume some normal physical activity after a few weeks. It was great! Unfortunately, it was also short lived. My symptoms of tachycardia came back after two months.
After ablation number three was unsuccessful, I was crushed. I truly think that Dr. Sakaguchi was crushed too, we had created this odd relationship because of my anomaly. I was broken, and he was really committed to fixing me. Every time we suffered a setback, I felt like we suffered it together.
My doctor and I talked about alternatives, and decided to try drug therapy for a while to see if it could be successful. I was going to continue meds, but at a higher dose and see if we could control the rhythm and fast heart rate that way. I had been on several different meds by this time, just in smaller quanitites. This round was Metoprolol, three times per day, a fairly normal amount to start, and typically well tolerated. The meds worked well at controlling my heart rate, I was exhausted but figured it was worth it. We had decided to try drug therapy for six months and then reassess if needed. I started going back to the gym, and took up running. It was nice to have some amount of normalcy again. About two months into it, I started to have side effects from the drugs. I was suffering from horrible depression that couldn’t be ignored, and luckily it was my pharmacist at Target that told me it was probably a side effect of the heart drug. She told me to contact my doctor immediately , which I did. He immediately took me off of the metoprolol and placed me back on to a low dose of atenolol in the winter of 2006.
My doctor was conservative when it came to ablating again. I had already been through three ablations, all of which has been more than 10 hours each. My body needed time to recuperate from the procedure itself and from the radiation that I had been exposed to. We now had to be careful of how much exposure I got to x-rays. I tolerated the drug therapy at the low dose, but the issue was that it wasn’t enough to control the rate, so I was basically tachycardic and horribly dizzy whenever the meds wore off. We tried yet another ablation at the U of MN in May of 2007. This time when they sedated me, my tachycardia played hide and seek. It completely disappeared! So ablation number four was a wash out too. No response to pacing, no burning.. no chance of success even close. I was completely losing hope.
We continued with the drug therapy for quite some time, me on the low dose that I could tolerate, but tachycardic much of the time. In addition to the tachycardia, I was very dizzy too. Although I didn’t have any more epoisodes of syncope, it really was from sheer will. I would force myself to remain awake and aware when it happened. I would basically will myself to keep some glimmer so that I didn’t pass out. I continued like this until the fall of 2008, when I just couldn’t take it anymore. I was living my life feeling terrible all the time, and it just wasn’t worth it.
My doctor contacted C.A.R.I. once again and talked to another doctor about doing an ablation. Dr. Jackman had since left to do other work for the private sector, so I would be a patient of Dr. Sunny Po. Dr. Po agreed to see me in OK City in November of 2008. Dr. Po called me about a week before I was scheduled to go to C.A.R.I. to talk about the procedure. He expressed concern that my arrhythmia has disappeared in the previous ablation due to the sedative use. He asked me if I would be open to having the procedure completely without sedation. He asked if I was “strong of mind” and able to find “my happy place”. I assured him that I felt like I was strong and capable. The idea of going through the ablation without drugs seemed like a daunting task. I had no idea what I would feel or if I would be in pain, but once again it seemed like it would be worth it if it was successful, and I was willing to do just about anything to feel better.
I arrived in OK City before Thanksgiving, and underwent the ablation, what I termed Lucky Number Five. To be frank, it was the most horrible experience of my life. Even though there are no nerve endings inside the heart, I could feel them burning me. I thought I was dying, there was so much pressure and pain in my chest. At a few points I know I screamed from the pain, and of course I was in sobbing uncontrollably. I tolerated the pain for as long as I could, and when they thought they had the tachycardia identified, they finally sedated me. I woke up after a relatively short procedure, this one only lasting six hours. They told me that it appeared I was finally cured. Dr. Po commented after the procedure that this was the most challenging case he had ever had while practicing. I was extremely happy with my result, and because I had little sedation during the procedure, my recovery was really fast. I was trucking around the nurses station the next morning, bugging them to let me go. I felt really great and traveled home to Minnesota to resume my life.
I’m sure you’ll find this a huge surprise, but my results were once again short lived. After about a month I started to have a fast heart rate again. I returned to the doctor for a check up and my resting heart rate was 123. I was panicked! He asked me to wait just a couple more weeks to see if it slowed down on its own, maybe it was just stress or anxiety. I returned at a follow up visit and the rate was still high, it was time to talk about more extreme measures. My doctor and I talked again about the idea of a pacemaker. We had this conversation a few times over the last few years, but had always dismissed it as being too radical. This time was different. I think this time he knew I was at the end of my rope, I was desperate for a solution.
I couldn’t take meds at a level that would work to control the heart rate. I had already have five ablations and would never be able to have any more. As a result of those ablations, I had been exposed to too much radiation and now needed to be checked for melanoma periodically. We decided that a pacemaker was probably the only option left for a normal slow heart rhythm and a chance at a normal life.
So this brings us to real time-
On Friday 2/6/09 (also the American Heart Associations day for Go Red for Women) I will be admitted to the hospital for one last ablation and the implantation of a pacemaker. They will sedate me, place catheters as they have so many times before, and then burn my AV Node beyond recognition. This burning will block the AV Node from sending any signals correct or incorrect. The pacemaker will be implanted to pace my heart 100% of the time . I consider myself lucky, I was admitted to a pacemaker study sponsored by Medtronic, so I will get a state of the art model called the Consulta. As the gentleman on the Medtronic phone line said, “It’s got all the bells and whistles”. So, please check back in.. I hope to have good news to report in a few days.
Hopeful once again,
Lea

My New Pacemaker
 I have a model called the Insync III, and before you ask- no it doesn’t make me a better dancer. The Insync III is a pacemaker that is used for Cardiac Resynchronization Therapy (CRT) and is a bi-ventricular model. Basically that just means that the device can be programmed to have a high and low limit and has three wires leading into my heart instead of two. Right now my pacemaker is set for a minimum of 80 beats per minute, and a maximum of 120 beats per minute. To put a little context behind that, 80 BPM is like Marcy Playground, Sex & Candy and 120 BPM is more like Limp Bizkit, Nookie. I’m currently hovering at about 85 BPM most of the time which is like Alanis Morrisette, Ironic.
I have a model called the Insync III, and before you ask- no it doesn’t make me a better dancer. The Insync III is a pacemaker that is used for Cardiac Resynchronization Therapy (CRT) and is a bi-ventricular model. Basically that just means that the device can be programmed to have a high and low limit and has three wires leading into my heart instead of two. Right now my pacemaker is set for a minimum of 80 beats per minute, and a maximum of 120 beats per minute. To put a little context behind that, 80 BPM is like Marcy Playground, Sex & Candy and 120 BPM is more like Limp Bizkit, Nookie. I’m currently hovering at about 85 BPM most of the time which is like Alanis Morrisette, Ironic.